Exploring the Benefits of Simulators in Medical Education for Heart and Lung Auscultation and Trauma Care
In today's rapidly evolving medical field, the integration of technology has revolutionized medical education. One notable advancement is the use of simulators for training in heart and lung auscultation and trauma care. Simulators offer a hands-on, interactive experience that bridges the gap between theory and practice, providing students with a realistic environment to develop and refine their skills.
With the ability to replicate a wide range of clinical scenarios, simulators offer a safe and controlled setting for students to learn and master complex procedures. By providing immediate feedback, simulators allow learners to identify and correct their mistakes, enhancing their diagnostic abilities and critical thinking skills.
Moreover, simulators enable educators to tailor training sessions to each individual student's needs, facilitating personalized learning experiences. This technology can significantly reduce the time required for students to become proficient in auscultation and trauma care, ultimately improving patient outcomes.
Through this article, we will explore the myriad benefits of simulators in medical education for heart and lung auscultation and trauma care. We will delve into the ways in which simulators enhance learning, empower students, and ultimately contribute to the advancement of medical practice.
Join us as we uncover the transformative potential of simulators in elevating medical education to new heights.
Importance of simulators in medical education
Medical education is a complex and demanding field that requires continuous innovation to keep up with the evolving healthcare landscape. Simulators have emerged as a valuable tool in medical education, offering numerous benefits for both students and educators.
One of the primary advantages of using simulators is the ability to create realistic clinical scenarios. Simulators can replicate a variety of heart and lung conditions, allowing students to practice auscultation in a controlled environment. This hands-on experience enables learners to gain confidence and familiarity with different sounds, improving their diagnostic accuracy.
Simulators also provide immediate feedback, which is invaluable for learning and skill development. Students can receive instant information about the correctness of their diagnosis, allowing them to make adjustments and learn from their mistakes. This feedback loop promotes critical thinking and enhances the learning process.
Asucultation simulator offer a safe learning environment. Medical procedures can be risky, especially for beginners. Simulators provide a risk-free space where students can make errors without compromising patient safety. This safety net allows learners to experiment, explore different approaches, and develop their skills without fear of consequences.
Incorporating simulators into medical education programs also helps address the scarcity of clinical training opportunities. With limited patient cases available for practice, simulators offer an alternative solution. Students can access a wide range of simulated scenarios, ensuring they have sufficient exposure to different conditions and procedures.
Simulators play a crucial role in medical education by providing realistic clinical scenarios, immediate feedback, a safe learning environment, and expanded training opportunities. These advantages contribute to improved learning outcomes and better-prepared healthcare professionals.
Simulators for heart and lung auscultation
Heart and lung auscultation is a fundamental skill for healthcare practitioners, especially those specializing in cardiology and respiratory medicine. Simulators designed for auscultation training offer a unique opportunity to develop and refine this skill in a controlled environment.
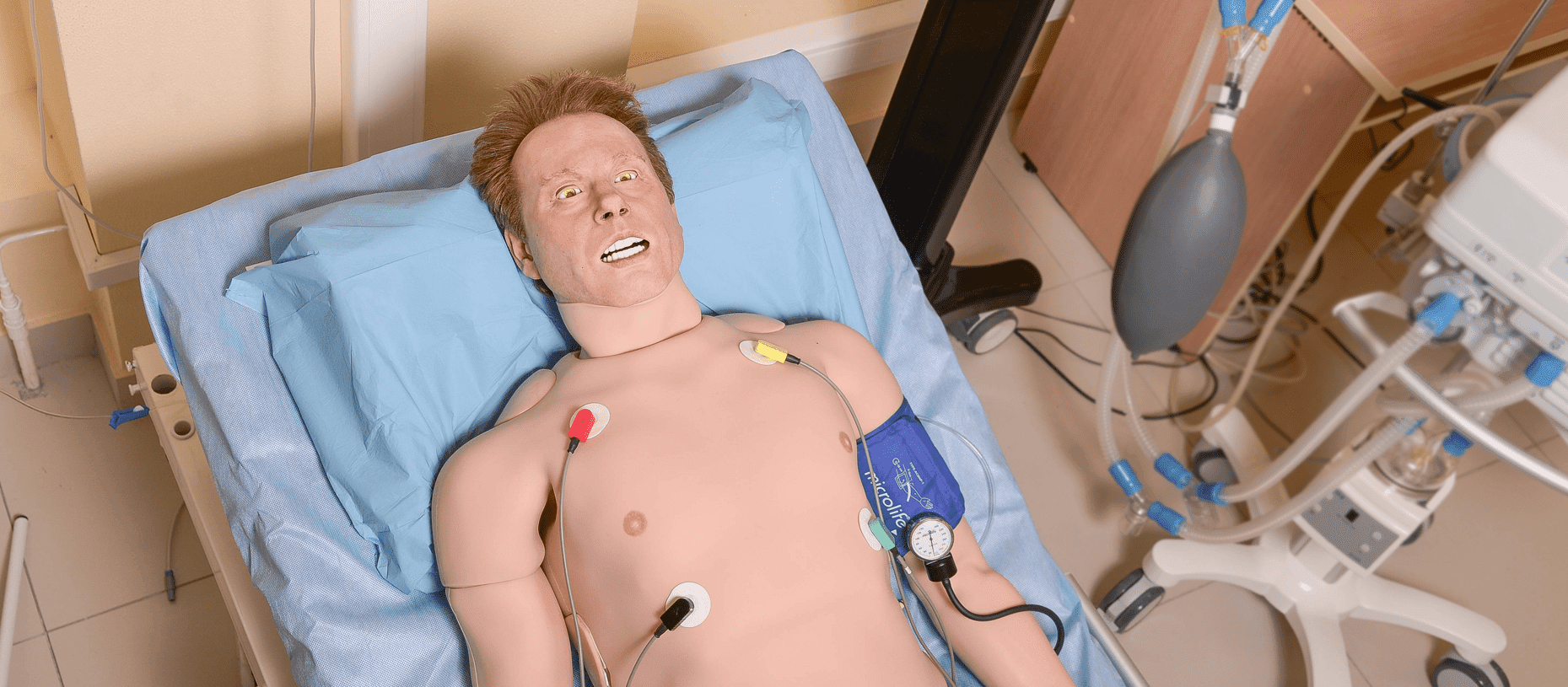
Simulators for heart and lung auscultation typically consist of anatomically accurate manikins equipped with speakers that produce realistic heart and lung simulator sounds. These simulators allow students to practice auscultation techniques using stethoscopes, just as they would in a clinical setting.
One significant advantage of using simulators for auscultation training is the ability to replicate a wide range of heart and lung conditions. Students can encounter various murmurs, abnormal heart sounds, and respiratory patterns, providing a comprehensive learning experience. This exposure to diverse cases helps learners build a robust foundation in auscultation and prepares them for real-world patient encounters.
Simulators also enable students to develop the skill of differentiating between normal and abnormal sounds. By repeatedly practicing on simulators, learners become proficient in identifying subtle variations in heart and lung sounds, improving their diagnostic accuracy. This skill is essential for early detection and appropriate management of cardiovascular and respiratory conditions.
Additionally, simulators offer the opportunity for repetition and deliberate practice. Students can practice auscultation techniques as many times as needed, allowing them to refine their skills and build muscle memory. This repetition is crucial for mastery and ensures that students are well-prepared to recognize and interpret auscultatory findings in actual patient encounters.
It is worth noting that simulators for heart and lung auscultation are often accompanied by visual aids, such as waveform displays and anatomical diagrams. These visuals help students correlate the sounds they hear with the underlying physiological processes, deepening their understanding of cardiac and respiratory anatomy and pathology.
In conclusion, simulators for heart and lung auscultation provide a realistic and comprehensive learning experience. They enable students to encounter a wide range of clinical cases, develop the skill of differentiating between normal and abnormal sounds, practice repetition and deliberate practice, and deepen their understanding of cardiac and respiratory anatomy. By incorporating medical simulator into auscultation training, medical education programs can equip students with the necessary skills to excel in their clinical practice.
Benefits of using simulators for heart and lung auscultation training
The use of simulators for heart and lung auscultation training offers numerous benefits for students, educators, and patients alike. Let's explore some of these advantages in detail.
Firstly, simulators provide a safe and controlled learning environment for students. Unlike real patients, simulators do not experience pain or discomfort. This allows learners to focus on the task at hand without worrying about causing harm. The absence of risk creates a stress-free environment, enabling students to practice and explore different auscultation techniques without fear or hesitation.
Simulators also offer immediate feedback, which is crucial for skill development. Students can receive real-time information about the accuracy of their diagnoses, allowing them to make corrections and refine their approach. This feedback loop fosters self-reflection, critical thinking, and continuous improvement, all of which are vital for becoming competent healthcare practitioners.
Furthermore, simulators enhance the efficiency of training programs by reducing the time required for students to become proficient in auscultation. Traditional methods of learning auscultation, such as relying solely on patient encounters, can be time-consuming and unpredictable. Simulators provide a consistent and readily available resource for practice, ensuring that students receive sufficient training to develop their skills efficiently.
Another benefit of using simulators for auscultation training is the ability to customize learning experiences. Educators can tailor scenarios to meet the specific needs of individual students, allowing them to focus on areas where they need improvement. This personalized approach enhances the effectiveness of training and ensures that students receive targeted instruction.
Additionally, simulators facilitate the integration of technology into medical education. With the advancement of digital health, simulators can be connected to virtual platforms, allowing for remote learning and assessment. This flexibility enables students to access training resources from anywhere, at any time, increasing accessibility and expanding educational opportunities.
In summary, the benefits of using simulators for heart and lung auscultation training are manifold. They provide a safe learning environment, offer immediate feedback, enhance training efficiency, facilitate personalized learning experiences, and enable the integration of technology into medical education. By harnessing these advantages, medical education programs can equip students with the skills and knowledge necessary for excellent patient care.
Simulators for trauma care
Trauma care is a critical aspect of medical practice, as it involves the immediate management of life-threatening injuries. Simulators designed for trauma care training offer a realistic and immersive experience that prepares students for high-pressure situations.
Trauma simulators often consist of manikins with simulated injuries, such as wounds, fractures, and burns. These simulators can replicate a variety of trauma scenarios, ranging from minor injuries to severe emergencies. This diversity allows students to practice the full spectrum of trauma care, from basic wound dressing to advanced life support techniques.
One significant advantage of using simulators for trauma care simulator training is the ability to create realistic and dynamic scenarios. Simulators can simulate bleeding, breathing difficulties, and other physiological responses to trauma, providing an immersive experience for students. This realism helps learners develop the necessary skills to assess and manage trauma patients effectively.
Simulators also offer the opportunity for team-based training. Trauma care often involves a multidisciplinary approach, requiring effective communication and coordination among healthcare professionals. Simulators can facilitate collaborative learning by allowing students from different disciplines to work together in simulated trauma scenarios. This teamwork training enhances interprofessional collaboration and prepares students for real-world trauma care situations.
Additionally, simulators provide students with the opportunity to practice critical decision-making under pressure. Traumatic injuries require quick thinking and rapid decision-making to ensure the best possible outcome for the patient. By exposing students to realistic trauma scenarios, simulators help develop their ability to prioritize and make effective decisions in high-stress situations.
Furthermore, simulators allow for the repetition of procedures and techniques. Students can practice trauma interventions multiple times, refining their skills and building confidence. This repetition is crucial for mastery and ensures that students are well-prepared to provide efficient and timely care to trauma patients.
In conclusion, simulators for trauma care training offer a realistic and immersive learning experience. They enable students to encounter a wide range of trauma scenarios, practice team-based training, develop critical decision-making skills, and engage in repetition and deliberate practice. By incorporating simulators into trauma care training, medical education programs can prepare students to deliver effective and efficient care in high-pressure situations.
Advantages of using simulators for trauma care training
The use of simulators for trauma care training provides several advantages that contribute to better-prepared healthcare professionals and improved patient outcomes. Let's explore some of these advantages in more detail.
Firstly, simulators offer a safe learning environment for trauma care training. Simulated trauma scenarios allow students to practice without the risk of causing harm to real patients. This safety net encourages students to take risks, make mistakes, and learn from them, all of which are essential for skill development and proficiency in trauma care.
Simulators also provide immediate feedback during trauma care training. Students can receive real-time information about the effectiveness of their interventions, allowing them to make adjustments and improve their techniques. This instant feedback fosters reflective practice and continuous improvement, ensuring that students develop the necessary skills to provide optimal care to trauma patients.
Furthermore, simulators enhance the efficiency of trauma care training programs. Traditional methods of learning trauma care, such as relying solely on real patient encounters, can be limited by the availability and variability of trauma cases. Simulators provide a consistent and standardized resource for practice, ensuring that students receive sufficient training to develop their skills efficiently.
Another advantage of using simulators for trauma care training is the ability to create challenging and realistic scenarios. Simulators can replicate complex trauma situations that may be difficult to encounter in real-life practice. This exposure to diverse and challenging cases prepares students for a wide range of trauma scenarios, enabling them to respond effectively to any situation they may encounter in their future careers.
Furthermore, simulators allow educators to assess students' performance objectively. By monitoring students' actions and decisions during simulated trauma scenarios, educators can identify areas for improvement and provide targeted feedback. This assessment process ensures that students are competent and well-prepared to deliver high-quality trauma care.
In summary, the advantages of using simulators for trauma care training are significant. They provide a safe learning environment, offer immediate feedback, enhance training efficiency, create challenging and realistic scenarios, and enable objective assessment. By leveraging these advantages, medical education programs can equip students with the skills and confidence necessary to provide optimal care to trauma patients.
Best practices for incorporating simulators into medical training programs
The successful integration of simulators into auscultation manikins training programs requires careful planning and implementation. Here are some best practices to consider when incorporating simulators into medical education:
Needs assessment: Before introducing simulators, conduct a needs assessment to identify specific areas where simulators can enhance training. Determine the learning objectives and competencies that simulators can address, ensuring alignment with the curriculum and desired learning outcomes.
Faculty training: Provide comprehensive training for educators on how to effectively utilize simulators in teaching. Educators should be familiar with simulator functionalities, scenario design, and debriefing techniques. Ongoing professional development opportunities should be available to ensure educators stay up-to-date with the latest advancements in simulation-based education.
Scenario design: Develop realistic and relevant scenarios that align with the intended learning objectives. Consider the complexity and progression of scenarios, ensuring they cater to learners at different stages of training. Collaborate with subject matter experts to ensure the accuracy and authenticity of simulated scenarios.
Debriefing: Incorporate structured debriefing sessions into simulation-based training. Debriefing allows students to reflect on their performance, identify areas for improvement, and receive feedback from educators. Follow established debriefing models, such as the Advocacy-Inquiry or Plus-Delta approach, to facilitate effective and constructive discussions.
Integration with the curriculum: Integrate simulators into the existing curriculum to enhance learning and complement other educational activities. Ensure that simulator-based training aligns with other teaching methods and assessments, creating a cohesive and comprehensive learning experience for students.
Assessment and evaluation: Develop robust assessment strategies to evaluate students' performance during simulator-based training. Utilize a combination of formative and summative assessments to measure students' knowledge, skills, and attitudes. Regularly review and refine assessment tools to ensure their validity and reliability.
Research and innovation: Encourage research and innovation in simulation-based education. Collaborate with researchers to explore the effectiveness of simulators in achieving desired learning outcomes. Stay informed about the latest advancements in simulation technology and incorporate innovative approaches into training programs.
By following these best practices, medical education programs can maximize the benefits of simulators and create a rich and effective learning environment for students.


Comments
Post a Comment